Starting January 1, 2026, Indiana Medicare Supplement policyholders age 65 and older will have an annual 60-day guaranteed issue period beginning on their birthday.
Applications using this new guaranteed issue right can be signed starting January 1, 2026.
Note: For commission-related questions, please check your agent portal. For any future commission changes, the carrier will email you so keep an eye on your inbox.
The Birthday Rule allows Medicare Supplement members to change carriers while keeping their existing plan type, without medical underwriting. This means your clients can shop for better rates or service without worrying about health questions.
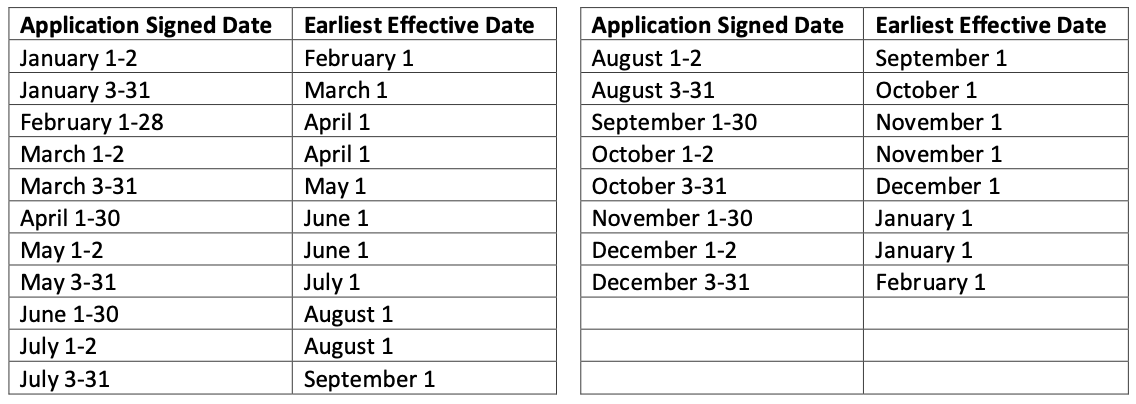
Coverage becomes effective on the first day of the month following the member's birthday, and clients have 60 days from their birthday to make the switch.
Your clients must keep the same Medicare Supplement plan letter (for example, Plan G to Plan G or Plan N to Plan N). They cannot change to a different plan type using this guaranteed issue right. This varies from state to state so please remember we are only talking about Indiana here.
If a client wants to switch to a different plan letter, they'll need to complete the health history section and pass medical underwriting.
We'll update this announcement as we recieve more communications from carriers.
But we do have some instructional information to share from both Humana and Anthem.
Humana:
Anthem Instructions: The Birthday Rule appears as GI Right #9 on updated paper applications available in enrollment kits on Storefront. Electronic enrollment applications will be updated November 15th.
Cigna Instructions: Commissions for Indiana Birthday Rule will be the same as Open Enrollment/Underwriting, as required by the state. View Cigna's complete Guaranteed Issue Rights guide for more detailed information.
INA Instructions: Applications applying under the Birthday Rule can be signed 1/1/2026 and later when the rule goes into effect. The effective date can be up to 60 days after the applicant's birthday but must be on the first of the month. Required proof includes a copy of the personalized policy/certificate schedule page or ID card showing the policyholder's name and plan.
Wellabe/Medico Instructions: Starting with applications dates 1/1/2026 and later when the birthday rule goes into effect, enrollment platforms will be updated with an additional question “Are you in a Special Enrollment Period?” If electing to use the Special Enrollment Period, mark Yes to this question and No to Open Enrollment and Guarantee Issue coverage. Please refer to the agent underwriting guide and agent portal for more detailed information on the birthday rule and commission information.
Mutual of Omaha:
WoodmenLife:
American Benefit Life: